ISCHEMIC HEART DISEASE AND ANESTHESIA

The aging of the population increases the likelihood that patients undergoing surgery will have coexisting ischemic heart disease. Angina pectoris, acute myocardial infarction, and sudden death are often the first manifestations of this disease. Cardiac dysrhythmias are the major cause of sudden death. The two most important risk factors for the development of coronary artery atherosclerosis are male gender and increasing age. Additional risk factors include hypercholesterolemia, hypertension, cigarette smoking, diabetes mellitus, obesity, a sedentary lifestyle, and a family history of premature development of ischemic heart disease. Psychological factors such as type A personality and stress have also been implicated. Patients with ischemic heart disease can present with chronic stable angina or with acute coronary syndrome. The latter includes ST elevation myocardial infarction (STEMI) on presentation and unstable angina/non–ST elevation myocardial infarction (UA/ NSTEMI).
PREOPERATIVE EVALUATION
The preoperative history is meant to elicit the severity, progression, and functional limitations imposed by ischemic heart disease. It should focus on determining the presence of major,moderateandminorclinicalriskfactorsinaparticular patient. Myocardial ischemia, left ventricular dysfunction, and cardiac dysrhythmias are usually responsible for the signs and symptoms of ischemic heart disease. Symptoms such as angina and dyspnea may be absent at rest, emphasizing the importance of evaluating the patient’s response to various physical activities such as walking or climbing stairs. Limited exercise tolerance in the absence of significant lung disease is very good evidence of decreased cardiac reserve. If a patient can climb two to three flights of stairs without symptoms, it is likely that cardiac reserve is adequate. Dyspnea after the onset of angina pectoris suggests the presence of acute left ventricular dysfunction due to myocardial ischemia. It is important to recognize the presence of incipient congestive heart failure preoperatively because the added stresses of anesthesia, surgery, fluid replacement, and postoperative pain may result in overt congestive heart failure.
Key points in the history
-
Identify serious cardiac conditions such as unstable coronary syndromes, prior angina, recent or past MI, decompensated heart failure, significant arrhythmias, and severe valvular disease
-
Determine whether the patient has a prior history of a pacemaker or implantable cardioverter defibrillator (ICD) or a history of orthostatic intolerance
-
Modifiable risk factors for coronary heart disease
-
Patient’s functional capacity (assessment of an individual’s capacity to perform a spectrum of common daily tasks)
-
Evidence of associated diseases, such as peripheral vascular disease, cerebrovascular disease, diabetes mellitus, renal impairment, and chronic pulmonary disease
-
In patients with established cardiac disease, any recent change in symptoms
-
Current medications used, including herbal and other nutritional supplements, and dosages
-
Use of alcohol, tobacco, and over-the-counter and illicit drugs
Age and Gender
Advanced age is a special risk because:
a. Increased likelihood of coronary disease
b. Effects of aging on the myocardium
c. Mortality of acute MI increases dramatically in the aged
d. Intraoperative or perioperative MI has a higher mortality in the aged
Gender is important because:
a. Premenopausal women have a lower incidence of CAD
b. In general, symptomatic CAD occurs 10 or more years later in women than in men. (women who have premature menopause, such as after oophorectomy, are an exception to this rule.)
c. Women with diabetes mellitus have an increased risk that is equivalent to men of the same age
d. Mortality rate after acute MI is greater for women than for men, but older age and diabetes mellitus account for
much of this difference.
Physical examination
-
General appearance—Pallor, cyanosis, dyspnea during conversation or with minimal activity, Cheyne-Stokes respiration, poor nutritional status, obesity, skeletal deformities, tremor, and anxiety
-
Elevated jugular venous pressure Hepatojugular reflux
-
Peripheral edema
-
A cardiovascular examination should include an assessment of vital signs (including measurement of blood pressure in both arms), carotid pulse contour and bruits, jugular venous pressure and pulsations, auscultation of the lungs, precordial palpation and auscultation, abdominal palpation, and examination of the extremities for edema and vascular integrity. The presence of an implanted pacemaker or ICD can also be confirmed by physical examination.
Comorbid diseases
Comorbid diseases heighten the risk of anesthesia and may complicate cardiac management. The most common of these conditions are:
Pulmonary diseases — Either obstructive or restrictive pulmonary disease (Hypoxemia, hypercapnia, acidosis, and increased work of breathing can all lead to further deterioration of an already compromised cardiopulmonary system.)
Diabetes mellitus — Its presence should heighten suspicion of CAD, particularly because CAD and myocardial ischemia are more likely in patients with diabetes mellitus. Lee et al identified insulin treated diabetes as a significant risk factor for cardiac morbidity.
Renal impairment — Preexisting renal disease, i.e. preoperative serum creatinine levels 2 mg per dl or greater or reduced glomerular filtration rate has been identified as a risk factor for postoperative renal dysfunction and increased long-term morbidity and mortality.
Hematologic disorders — Anemia imposes a stress on the cardiovascular system that may exacerbate myocardial ischemia and aggravate heart failure. Polycythemia, thrombocytosis, and other conditions that increase viscosity and hypercoagulability may increase the risk of thromboembolism or hemorrhage.
Clinical assessment
The goals of preoperative assessment are to:
-
Identify the risk for heart disease based on risk factors
-
Identify the presence and severity of heart disease from symptoms, physical findings, or diagnostic tests
-
Determine the need for preoperative interventions
-
Modify the risk for perioperative adverse events
The presence of 1 or more of the following conditions mandates intensive management and may result in delay or cancellation of surgery unless the surgery is emergent. These include:
-
Unstable coronary syndromes—unstable or severe angina [Canadian Cardiovasular Society (CCS) class III or IV], recent MI (more than 7 days, but within 30 days)
-
Decompensated heart failure—New York Heart Association (NYHA) class IV; worsening or new onset heart failure
-
Significant arrhythmias—High-grade atrioven-tricular block; Mobitz II atrioventricular block; Third-degree atrioventricular heart block; Symptomatic ventricular arrhythmias; Supraventricular arrhythmias (including atrial fibrillation) with uncontrolled ventricular rate (HR > 100 bpm at rest); Symptomatic bradycardia; newly recognized ventricular tachycardia
-
Severe valvular disease—Severe aortic stenosis (mean pressure gradient > 40 mm Hg, aortic valve area < 1.0cm2, or symptomatic); Symptomatic mitral stenosis (progressive dyspnea on exertion, exertional presyncope, or heart failure)
Given the increasing use of the Revised Cardiac Risk Index3, the American College of Cardiology/American Heart Association (ACC/AHA) chose to replace the intermediate- risk category with the clinical risk factors from the index, with the exclusion of the type of surgery, which is incorporated elsewhere in the approach to the patient (Table 5.1).
A history of MI or abnormal Q waves by ECG is listed as a clinical risk factor, whereas an acute MI (defined as at least 1 documented MI 7 days or less before the examination) or recent MI (more than 7 days but less than or equal to 1 month before the examination) with evidence of important ischemic risk by clinical symptoms or noninvasive study is an active cardiac condition. This definition reflects the consensus of the ACC Cardiovascular Database Committee. In this way, the separation of MI into the traditional 3 and 6 month intervals has been avoided.4, 5 Current management of MI provides for risk stratification during convalescence.6 If a recent stress test does not indicate residual myocardium at risk, the likelihood of reinfarction after noncardiac surgery is low. Although there are no adequate clinical trials on which to base firm recommendations, it appears reasonable to wait 4 to 6 weeks after MI to perform elective surgery.
Minor predictors are recognized markers for cardiovascular disease that have not been proven to increase perioperative risk independently, for example, advanced age (> 70 years), abnormal ECG (LV hypertrophy, left bundle-branch block, ST-T abnormalities), rhythm other than sinus, and uncontrolled systemic hypertension. The presence of multiple minor predictors might lead to a higher suspicion of CAD but is not incorporated into the recommendations for treatment.

Simplified Cardiac Evaluation for Non-cardiac Surgery
Figure 5.1 depicts the cardiac evaluation algorithm proposed by ACC/AHA for noncardiac surgery.

The ACC/AHA algorithm encompasses patients with known IHD or associated risk factors who are having noncardiac surgery. The 2014 ACC/AHA guidelines define an emergency procedure as one where life or limb would be threatened if surgery did not proceed within 6 hours or less; an urgent procedure as one where life or limb would be threatened if surgery did not proceed within 6 to 24 hours; and a time-sensitive procedure as one where delays exceeding 1 to 6 weeks would adversely affect outcomes (e.g., most oncology surgery). Based on this classification scheme, patients should proceed directly to any required emergency surgery without further preoperative cardiac assessment. For these individuals, the focus should be on surveillance (e.g., serial cardiac enzymes, hemodynamic monitoring, serial ECGs) and early treatment of any postoperative cardiovascular complications.
In the second step, active cardiac conditions—such as acute coronary syndromes, decompensated heart failure, severe valvular disease (e.g., critical aortic stenosis), suspected significant pulmonary hypertension, or significant arrhythmias (e.g., atrial fibrillation with rapid ventricular rate, sustained ventricular tachycardia)—should be ruled out in patients not requiring emergency surgery. If any of these conditions are present, they must be initially treated, after which the original planned surgery can be reconsidered based on its risk-benefit balance. When assessing whether a patient has an active cardiac condition, the anesthesiologist should inquire about any recent myocardial infarction. The 2014 ACC/AHA guidelines recommend deferring nonurgent surgery until 60 days after a recent myocardial infarction.
In the third step, perioperative cardiac risk should be estimated based on readily available clinical information that encompasses both patient-level (e.g., comorbidities) and surgery-level (e.g., procedure type) characteristics. The 2014 ACC/AHA guidelines and 2014 ESC/ESA guidelines recommend using clinical risk indices, namely the Revised Cardiac Risk Index (RCRI), ACS NSQIP surgical risk calculator (https://riskcalculator.facs.org/RiskCalculator), or NSQIP Myocardial Infarction and Cardiac Arrest risk calculator. If these indices find the estimated risk of postoperative myocardial infarction or death to be less than 1% (consistent with RCRI ≤ 1), the ACC/AHA guidelines recommend that patients simply proceed directly to surgery.
In the fourth and subsequent steps, the ACC/AHA algorithm recommends that a patient with a functional capacity of 4 or more METs should proceed directly to surgery. The major clinical challenge with this recommendation pertains to how best to estimate patients’ preoperative functional capacity in clinical practice. Simple subjective assessment of functional capacity based on the usual pre-operative history does not accurately estimate true exercise capacity, and does not accurately predict postoperative cardiovascular complications. Thus, in clinical practice, anesthesiologists should generally use a structured questionnaire. If a patient is deemed to have either low (i.e., < 4 METs) or uncertain functional capacity, the AHA/ACC guidelines recommend consideration of exercise or pharmacologic cardiac stress testing, if the results could plausibly inform decision making or clinical care. Patients with high-risk abnormal test results can be considered for subsequent coronary angiography, and possibly revascularization (if usual nonoperative indications for coronary revascularization are met). Invasive coronary angiography is the gold standard for diagnosing IHD and may also be a follow-up option for patients with high-risk cardiac stress test results. During preoperative evaluation, the anesthesiologist should determine the presence, type (drug-eluting vs. bare-metal), location, and original indication of any coronary stent. Importantly, the ACC/AHA guidelines emphasize the importance of considering alternative less invasive or nonsurgical treatment for the underlying condition, especially in patients found to be at very high cardiac risk.

Canadian Cardiovascular Society (CCS) Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Non-cardiac Surgery
Strong recommendations included:
-
measuring brain natriuretic peptide (BNP) or N-terminal fragment of proBNP (NT-proBNP) before surgery to enhance perioperative cardiac risk estimation in patients who are 65 years of age or older, are 45-64 years of age with significant cardiovascular disease, or have a Revised Cardiac Risk Index score of 1 and above;
-
against performing preoperative resting echocardiography, coronary computed tomography angiography, exercise or cardiopulmonary exercise testing, or pharmacological stress echocardiography or radionuclide imaging to enhance perioperative cardiac risk estimation;
-
against the initiation or continuation of acetylsalicylic acid for the prevention of perioperative cardiac events, except in patients with a recent coronary artery stent or who will undergo carotid endarterectomy;
-
against alpha 2 agonist or beta-blocker initiation within 24 hours before surgery;
-
withholding angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker starting 24 hours before surgery;
-
facilitating smoking cessation before surgery;
-
measuring daily troponin for 48 to 72 hours after surgery in patients with an elevated NT-proBNP/BNP measurement before surgery or if there is no NT-proBNP/BNP measurement before surgery, in those who have a Revised Cardiac Risk Index score more than or equal to 1, age 45-64 years with significant cardiovascular dis- ease, or age 65 years or older; and
-
initiating of long-term acetylsalicylic acid and statin therapy in patients who suffer myocardial injury/infarction after surgery.

Duceppe, E., Parlow, J., MacDonald, P., Lyons, K., McMullen, M., Srinathan, S., … Devereaux, P. J. (2017). Canadian Cardiovascular Society Guidelines on perioperative cardiac risk assessment and management for patients who undergo noncardiac surgery. Canadian Journal of Cardiology, 33(1), 17–32. doi:10.1016/j.cjca.2016.09.008
BNP, brain natriuretic peptide; ECG, electrocardiogram; NT-proBNP, N-terminal pro-brain natriuretic peptide; PACU, postanesthesia care unit; PHTN, pulmonary hypertension; RCRI, Revised Cardiac Risk Index.
* Significant cardiovascular disease includes known history of coronary artery disease, cerebral vascular disease, peripheral artery disease, congestive heart failure, severe PHTN or a severe obstructive intracardiac abnormality (eg, severe aortic stenosis, severe mitral stenosis, or severe hypertrophic obstructive cardiomyopathy).
++Timing of surgery refers to emergency surgery (eg, severe trauma, ruptured aortic aneurysm), urgent surgery (eg, hip fracture, bowel obstruction), semiurgent surgery (eg, cancer with potential to metastasize), or elective surgery (eg, knee arthroplasty).
£ If physical examination suggests there is an unknown severe obstructive intracardiac abnormality (eg, severe aortic stenosis, severe mitral stenosis, or severe hypertrophic obstructive cardiomyopathy) or severe PHTN, then obtain an echocardiogram before surgery to inform the anesthesiologist, surgeon, and medical team of the type and degree of disease. If the history suggests the patient has an unstable cardiac condition (eg, unstable angina) then discussion with the patient and surgical/medical team is required to decide whether to delay, cancel, or proceed with surgery.
** Shared-care management refers to a multidisciplinary approach to inpatient postoperative care; this includes the surgeon and a medical specialist (eg, internist, cardiologist, gerontologist), who will help with perioperative monitoring and management of cardiovascular complications.

Surgery-specific Cardiac Risk Factors
The surgery- specific cardiac risk (Table 5.2) of non-cardiac surgery is related to 2 important factors. First, the type of surgery itself may identify a patient with a greater likelihood of underlying heart disease and higher perioperative morbidity and mortality. Perhaps the most extensively studied example is vascular surgery, in which underlying CAD is present in a substantial portion of patients. If the patient is undergoing vascular surgery, testing should only be considered if it will change management. Other types of surgery may be associated with similar risk to vascular surgery but have not been studied extensively. For nonvascular surgery, the degree of hemodynamic cardiac stress dictates the surgery-specific risk. Depending on the noncardiac surgical procedure, it may be associated with profound alterations in heart rate, blood pressure, vascular volume, pain, bleeding, clotting tendencies, oxygenation, neurohumoral activation, and other perturbations. The intensity of these coronary and myocardial stressors helps determine the likelihood of perioperative cardiac events. The perioperative morbidity related to the procedures ranges from 1% to 5%.
Table 5.2: Cardiac risk stratification for non-cardiac surgery
High risk procedures (reported cardiac risk >5%)
Aortic and other major vascular surgery
Peripheral vascular surgery
Intermediate risk procedures (reported cardiac risk 1-5%)
Intraperitoneal and intrathoracic surgery
Carotid endarterectomy
Head and neck surgery
Orthopedic surgery
Prostate surgery
Low risk procedures (reported cardiac risk <1%)
Endoscopic procedures
Superficial procedures
Cataract surgery
Breast surgery
Ambulatory surgery
Approach to patients with hypertension
As a universally measured variable with a recognized association with CAD, hypertension serves as a useful
marker for potential CAD. But numerous studies have shown that hypertension itself is not an independent
risk factor for perioperative cardiac events.In addition, several investigators have demonstrated exaggerated intraoperative blood pressure fluctuation with associated ECG evidence of myocardial ischemia in patients with
preoperative blood pressure elevation. This effect can be modified by treatment. Because intraoperative ischemia correlates with postoperative cardiac morbidity, it follows that control of blood pressure preoperatively may help reduce the tendency to perioperative ischemia.
Interestingly, patients with preoperative hypertension appear more likely to develop intraoperative hypotension than nonhypertensive persons; this is particularly true for patients taking angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonists. In some patients, this may be related to a decrease in vascular volume. In one report, intraoperative hypotension was associated with a greater incidence of perioperative cardiac and renal complications than intraoperative hypertension. Several authors have suggested withholding ACE inhibitors and angiotensin receptor antagonists the morning of surgery. Consideration should be given to restarting ACE inhibitors in the postoperative period only after the patient is euvolemic, to decrease the risk of perioperative renal dysfunction.
For stage 2 hypertension (Joint National Committee, JNC VII—systolic blood pressure greater than or equal to 160 mm Hg and diastolic blood pressure greater than or equal to 100 mm Hg), the potential benefits of delaying surgery to optimize the effects of antihypertensive medications should be weighed against the risk of delaying the surgical procedure. With rapidly acting intravenous agents, blood pressure can usually be controlled within a matter of several hours.
Approach to patients with heart failure
Heart failure (HF) has been identified in several studies as being associated with a poorer outcome when noncardiac surgery is performed. In a study by Goldman et al, both the presence of a third heart sound and signs of HF were associated with a substantially increased risk during noncardiac surgery. Detsky et al identified alveolar pulmonary edema as a significant risk factor, and Lee et al. also identified HF (defined as the presence of any of the following: history of congestive HF, pulmonary edema, or paroxysmal nocturnal dyspnea; physical examination showing bilateral rales or S3 gallop; or chest X-ray showing pulmonary vascular redistribution) as an independent predictor of risk. If possible, it is important to identify the cause of HF, because this may have implications concerning risk of death versus perioperative HF.
Preoperative noninvasive evaluation of Left ventricular (LV) Function
Resting LV function has been evaluated before noncardiac surgery by radionuclide angiography, echocardiography, and contrast ventriculography (Table 5.4).

Preoperative resting 12-Lead electrocardiogram
Class IIa Recommendation: (It Is reasonable to perform the procedure)
Preoperative resting 12-lead ECG is reasonable for patients with
known IHD,
significant arrhythmia,
peripheral arterial disease (PAD),
cerebrovascular disease (CVD), or
other significant structural heart disease
(except if undergoing low-risk surgical procedures).
Class IIb Recommendation: (The procedure may be considered)
Preoperative resting 12-lead ECG may be considered for asymptomatic patients without known coronary heart disease, except for those undergoing low-risk surgical procedures.
Class III Recommendation: (The procedure should not be performed because it is not helpful)
Routine preoperative resting 12-lead ECG is not useful for asymptomatic patients undergoing low-risk surgical procedures.
Note: Establishing a baseline for postoperative comparison is often the most important reason to obtain a preoperative ECG; however, this decision should be based on the patient’s likely risk of postoperative cardiovascular complications. Thus, a baseline ECG is unlikely to be helpful in an individual at very low risk for postoperative cardiac events. If a previous ECG is available from the previous 3 months and there has been no intervening change in clinical status, a repeat ECG is likely not needed.
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and manage- ment of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e278–e333.
Prognostic Gradient
Prognostic gradient of ischemic responses during an ECG-monitored exercise test in patients with suspected or proven CAD is summarised in Table 5.6.

Stress testing identifies CAD and its severity, but the positive predictive value for perioperative cardiac complications is generally only 5% to 25%. The negative predictive value of noninvasive tests for predicting perioperative events generally approaches 100%, so these tests are typically more informative about a patient who will not have an event than one who will.
Pharmacologic tests such as dobutamine echocardiography or nuclear perfusion imaging are necessary for patients unable to exercise, those with pacemakers or significant bradycardia, or those taking high dose b-adrenergic blockers.
A combination of exercise and imaging can be used in patients able to exercise who have significant abnormalities on the ECG that may interfere with the interpretation of ischemia via the ECG (e.g. LVH with a strain pattern, ST-T wave changes, or left bundle branch block [LBBB]).
Noninvasive Stress Testing Before non-cardiac surgery
Recommendations for noninvasive stress testing before noncardiac surgery are given in Table 5.7.

The two main techniques used in preoperative evaluation of patients undergoing noncardiac surgery who cannot exercise are to increase myocardial oxygen demand (by pacing or intravenous dobutamine) and to induce hyperemic responses by pharmacological vasodilators such as intravenous dipyridamole or adenosine. The most common examples presently in use are Dobutamine Stress Echocardiography (DSE) and intravenous dipyridamole/ adenosine myocardial perfusion imaging with both thallium 201 and technetium 99 m.
PREOPERATIVE MEDICATIONS
The preoperative period is an opportunity to identify patients with CAD who will benefit from long-term risk modification with statins, aspirin, exercise, and diet adjustment. Patients with symptoms consistent with ischemia (but without a diagnosis of CAD) or significant risk factors without medical management such as statins and aspirin may benefit from evaluation by a cardiologist regardless of whether they are having surgery. Preoperative evaluation should not simply focus on perioperative risk.
The only way known to increase oxygen supply to the myocardium of patients with coronary artery stenosis is to maintain diastolic BP, hemoglobin concentration, and oxygen saturation. The main goal of anesthesia practice for these patients has been to decrease the determinants of myocardial oxygen demand, heart rate, ventricular wall tension, and contractile performance and improve plaque stabilization. Thus, medical management designed to preserve all viable myocardial tissue may include the following:
-
Continuation of β-adrenergic receptor blocking drugs (propranolol, atenolol, esmolol, or metoprolol) to avoid β-blocker withdrawal leading to increased contractility and heart rate. The current ACC/AHA guidelines on perioperative b-blockade advocate that perioperative beta-blockade is a class I indication and should be used in patients previously taking b-blockers and those with a positive stress test undergoing major vascular surgery, although acute administration without titration may be associated with harm. Those already taking β-blockers need their dosages adjusted to achieve an HR lower than 70 beats/min if at all possible.
-
Vasodilation (with nitroglycerin or its “long-acting” analogs nitroprusside, hydralazine, or prazosin) to decrease ventricular wall tension may be beneficial, although there are currently no randomized trials that support the prophylactic use of these agents.
-
Aspirin, statins, exercise, and diet. These choices seem to be indicated in many patients. Strong consideration should be given to continuing aspirin perioperatively or discontinuing for the shortest duration possible if used for secondary prevention of vascular events. Algorithm for preoperative management of patients receiving antiplatelet therapy is given in figure 5.2.
-
Significant hypotension has been observed in patients treated long term with ACE inhibitors who undergo general anesthesia. Many recommend withholding ACE inhibitors for 24 hours before surgical procedures involving significant fluid shifts or blood loss. Hypotension attributable to ACE inhibitors is usually responsive to fluids or sympathomimetic drugs. If hypotension is refractory to these measures, treatment with vasopressin or one of its analogues may be required.
As a general rule, drugs given chronically (e.g.,antihypertensive medications and some ACE inhibitors) should be continued through the morning of surgery.

*High risk stents: long (>36 mm), proximal, overlapping or multiple stent implantation, stents for chronic total occlusions, stents in small vessels or bifurcated lesions.
**Examples of low risk situations: >3 months after BMS, stroke, uncomplicated MI, PCI without stenting.
***Risk of bleeding in closed space: Intracranial neurosurgery, intramedullary canal surgery, posterior eye
chamber ophthalmic surgery. In these situations, the risk/benefit ratio of upholding vs withdrawing aspirin
must be evaluated for each case individually, in case of aspirin upholding, early postoperative re-institution is important.
Abbreviations: MI, Myocardial infarction; ACS, Acute coronary syndrome; PAD, Peripheral artery disease; PCI, Percutaneous interventions; BMS, Bare metal stent; DES, Drug eluting stent
Role of Coronary Artery Bypass Graft or Percutaneous Coronary interventions before non-cardiac surgery
The following are the class I recommendations for coronary revascularization before non-cardiac surgery:
-
Stable angina who have significant left main coronary artery stenosis
-
Stable angina who have 3-vessel disease [particularly if Left Ventricular Ejection Fraction (LVEF) < 0.50]
-
Stable angina who have 2-vessel disease with significant proximal left anterior descending artery (LAD) stenosis and either ejection fraction (EF) less than 0.50 or demonstrable ischemia on noninvasive testing
-
High-risk unstable angina or non-ST segment elevation MI
-
Acute ST elevation MI
Patients undergoing elective noncardiac procedures who are found to have prognostic high risk coronary anatomy and in whom long-term outcome would likely be improved by coronary bypass grafting should generally undergo coronary revascularization before a noncardiac elective vascular surgical procedure or noncardiac operative procedures of intermediate or high risk. The cumulative mortality and morbidity of both the coronary revascularization procedure and the noncardiac surgery should be weighed carefully in light of the individual patient’s overall health, functional status, and prognosis.
Perioperative Percutaneous Interventions (PCI)
The present review of the literature suggests that PCI before noncardiac surgery is of no value in preventing perioperative cardiac events, except in those patients in whom PCI is independently indicated for an acute coronary syndrome.
For patients with stable coronary artery disease who undergo noncardiac surgery, Canadian Cardiovascular Society (CCS) recommend against preoperative prophylactic coronary revascularization. In the absence of clearly demonstrated benefit, the potential for surgical delays, increase in costs, and risk of bleeding with dual antiplatelet therapy supported a strong recommendation against prophylactic preoperative coronary revascularization.
In patients with CCS class III-IV or unstable angina, obtaining coronary revascularization before noncardiac surgery seems prudent; however, an individual risk-benefit assessment is required in patients who require urgent/semiurgent noncardiac surgery. Patients who receive PCI and a coronary stent should ideally have their noncardiac surgery delayed until the risks of stopping dual antiplatelet therapy are outweighed by the risks associated with delaying noncardiac surgery.
2016 guidelines published by the ACC/AHA recommend that elective noncardiac surgery should be delayed for 30 days or more after BMS implantation. In the case of DES, the ideal recommended minimum delay is 6 months. Based on expert opinion, the guidelines also indicate that elective noncardiac surgery can some- times be performed from 3 to 6 months after DES implantation (particularly with new generation stents), if the risk of stent thrombosis is judged to be less than the risk of further delaying surgery. When DAPT is temporarily interrupted before noncardiac surgery, the guidelines strongly recommend that aspirin be continued, and P2Y12 inhibitor therapy be restarted as soon as possible after surgery.

Prevention of Perioperative Myocardial Ischemia
Prevention of perioperative myocardial ischemia is essential to avoid the mechanical, metabolic, and electrophysiologic changes associated with acute imbalances in the relationship between myocardial oxygen supply and demand. Myocardial ischemia of sufficient severity or prolonged duration may result in reversible (e.g. myocardial stunning) or irreversible (e.g. infarction) damage, malignant ventricular arrhythmias, or cardiogenic shock. These potentially disastrous consequences are associated with high morbidity and mortality in patients with coronary artery disease.
Myocardial Oxygen Supply and Demand
The classical relationship between myocardial oxygen supply and demand indicates that when oxygen demand exceeds supply, the imbalance results in myocardial ischemia. Fortunately, this supply/demand relationship may be favorably altered by a variety of pharmacologic agents in the perioperative period to prevent the onset of myocardial ischemia. Such interventions should be aggressively undertaken in a manner equal to the vigilance required for the detection of acute ischemic events. Objectives of treatment include reducing demand for oxygen by myocardium at risk for development of ischemia while simultaneously increasing oxygen supply to this tissue.
Myocardial oxygen demand in the left ventricle is dependent on heart rate, myocardial contractility, and ventricular loading conditions. Heart rate is the most important of all physiologic factors that can be altered to reduce demand. Increases in heart rate not only lead to profound increases in oxygen consumption but also jeopardize perfusion in regions distal to coronary artery stenoses by reducing the duration of diastole. These actions are most pronounced in the left ventricular subendocardium. As stenosis severity increases, and with it the risk of ischemia and infarction, the role of coronary perfusion pressure (the difference between aortic diastolic and left ventricular end-diastolic pressures) gains greater significance. Myocardial blood flow is autoregulated to a relatively constant level under normal conditions, but the ability of the distal coronary vascular bed to dilate in response to increasing stenosis severity will eventually become exhausted. Finally, in the presence of severe stenosis, autoregulation fails to maintain coronary blood flow, and perfusion to the affected territory becomes directly dependent on coronary perfusion pressure. Deleterious increases in myocardial contractility and oxygen use may occur during the perioperative period because of β1-adrenoceptor stimulation by endogenous catecholamines. Left ventricular preload and afterload also affect myocardial oxygen demand by altering end-diastolic and end-systolic wall tension, respectively.
Many other factors, such as blood rheology, hematocrit, and coronary collateral blood flow, influence the myocardial oxygen supply/demand relationship as well. The degree to which any of these factors may result in myocardial ischemia is specific for each patient. Small decreases in coronary perfusion pressure or increases in heart rate may produce detrimental effects depending on the specific degree of coronary artery disease.

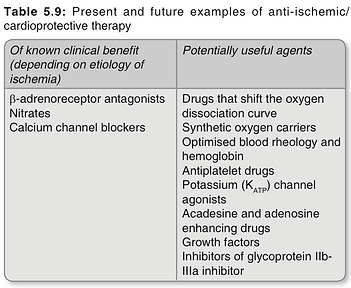
Traditional pharmacologic approaches to the prevention and treatment of ischemia focus on the oxygen supply/ demand relationship; however, novel therapeutic strategies are being studied intensively. Newer modalities may alter myocardial oxygen demand at the cellular or mitochondrial level independent of systemic and coronary hemodynamics. A list of potentially useful drugs and techniques (some of which are as yet only experimental) is shown in Table 5.9. It is important to recognize that no single method of treatment is ideal for all patients because of the multifactorial basis of myocardial ischemia. Furthermore, all therapeutic approaches have limitations, and the cost and benefit of each requires careful evaluation. However, for the vast majority of patients with coronary artery disease undergoing anesthesia, prevention of myocardial ischemia affords a benefit that greatly outweighs the potential cost of an ischemic episode.
Pharmacological preconditioning with volatile anesthetics, or anesthetic-induced preconditioning (APC), is a phenomenon whereby a brief exposure to volatile anesthetic agents protects the heart from the potentially fatal consequences of a subsequent prolonged period of myocardial ischemia and reperfusion. Although not completely elucidated, the cellular and molecular mechanisms of APC appear to mimic those of ischemic preconditioning, the most powerful endogenous cardioprotective mechanism. APC is mediated by adenosine triphosphate–dependent potassium channel activation in cardiac myocytes via a mechanism similar to that observed during ischemic preconditioning. Preliminary clinical evidence for anesthetic-induced preconditioning does not yet exist. Only preliminary results of one study have recently been reported. Volatile anesthetics may prove to be useful in patients with coronary artery disease provided that the relationship between myocardial oxygen supply and demand is not adversely affected.
MANAGEMENT OF ANESTHESIA IN PATIENTS WITH KNOWN OR SUSPECTED ISCHEMIC HEART DISEASE UNDERGOING NON-CARDIAC SURGERY
Goals for the perioperative management of patients with coronary artery disease include:
-
Prevent increases in sympathetic nervous system activity: Reduce anxiety preoperatively; prevent stress response and release of catecholamines by appropriate use of opioids or volatile anesthetics and b-adrenoceptor antagonists.
-
Decrease heart rate: Reduction in heart rate increases oxygen supply to ischemic myocardium and reduces oxygen demand; the use of β-blockers is the most effective means to reduce or attenuate deleterious increases in heart rate.
-
Preserve coronary perfusion pressure: Decreases in diastolic arterial pressure in the presence of severe coronary artery stenoses will lead to decreases in blood flow; preservation of perfusion pressure by administration of fluid or phenylephrine or a reduction in anesthetic concentration may be critical.
-
Decrease myocardial contractility: Reduces myocardial oxygen demand and can be accomplished with b-adrenoceptor antagonists or volatile anesthetics.
-
Precondition myocardium against stunning and infarction: In the future, this may accomplished by stimulating the adenosine triphosphate–dependent potassium channel with agents such as volatile anesthetics and opioid β-receptor agonists.
Premedication
Patients with known or suspected ischemic heart disease should receive good sedative/anxiolytic premedication. Cautious premedication may be advisable for patients with poor cardiopulmonary reserve. Perioperative strategies for continuation of other medications is discussed already.
Selection of anesthetic technique
Considerable debate still remains over the advantages and disadvantages of regional compared with general anesthesia for the patient with coronary artery disease. Unfortunately, no definitive study has proven that one approach (regional vs general anesthesia) is superior to the other. The advantages of regional anesthesia include greater reduction of intraoperative stress response, a reduction in hypercoagulability and thrombotic events, better quality of analgesia extending into postoperative period. A major potential problem of regional anesthesia in patients with coronary artery disease is a decrease in coronary perfusion pressure resulting from a reduction in sympathetic nervous system tone to the venous and arterial vasculature. Prompt treatment of hypotension that exceeds 20% of the preblock blood pressure is necessary. Likewise, potential shortcomings of general anesthesia comprise of the stress of tracheal intubation and emergence from anesthesia which can result in large increases in sympathetic nervous system stimulation that may produce unacceptable increases in heart rate, myocardial contractility, and left ventricular afterload. Volatile anesthetics alone antagonize adrenergic responses to stress, and these agents are even more effective in the presence of small doses of opioids. However, the incidence of postoperative cardiac morbidity and mortality does not appear to be significantly different between general and regional anesthesia.
It is important to avoid persistent and excessive changes in heart rate and systemic blood pressure. However, many episodes of intraoperative myocardial ischemia occur in the absence of hemodynamic changes. These episodes of myocardial ischemia may be due to regional decreases in myocardial perfusion and oxygenation. It is unlikely that this form of ischemia can be prevented by the anesthesiologist.
Particular attention should, however, be directed to control of the hemodynamic changes associated with the following interventions:
-
induction of anesthesia
-
laryngoscopy and tracheal intubation
-
surgical incision and stimulation
-
emergence from anesthesia
-
tracheal extubation.
Induction of anesthesia
Induction of anesthesia in patients with ischemic heart disease can be accomplished with an intravenous induction drug. Ketamine is not a likely choice because the associated increase in heart rate and systemic blood pressure transiently increases myocardial oxygen requirements. Tracheal intubation is facilitated by administration of succinylcholine or a nondepolarizing muscle relaxant.
Myocardial ischemia may accompany the sympathetic nervous system stimulation that results from direct laryngoscopy and tracheal intubation. Short-duration direct laryngoscopy (≤ 15 seconds) is useful in minimizing the magnitude and duration of the circulatory changes associated with tracheal intubation. If the duration of direct laryngoscopy is not likely to be brief or if hypertension already exists, it is reasonable to consider administering drugs to minimize the pressor response. Laryngotracheal lidocaine, intravenous lidocaine, esmolol, and fentanyl have all been shown to be useful for blunting the increase in heart rate evoked by tracheal intubation.
Maintenance of anesthesia
Intraoperative events associated with persistent tachycardia, systolic hypertension, sympathetic nervous system stimulation, arterial hypoxemia, or hypotension can adversely affect the patient with ischemic heart disease (Table 5.10). It is important to avoid persistent and excessive changes in heart rate and systemic blood pressure.

In patients with normal left ventricular function, tachycardia and hypertension are likely to develop in response to intense stimulation, as during direct laryngoscopy or painful surgical stimulation. Controlled myocardial depression using a volatile anesthetic may be useful in such patients to minimize the increase in sympathetic nervous system activity. The volatile anesthetic may be administered alone or in combination with nitrous oxide. Equally acceptable for maintenance of anesthesia is use of a nitrous oxide–opioid technique with the addition of a volatile anesthetic to treat any undesirable increases in blood pressure that accompany painful surgical stimulation. Overall, volatile anesthetics may be beneficial in patients with ischemic heart disease by virtue of decreasing myocardial oxygen requirements and preconditioning the myocardium to tolerate ischemic events, or they may be detrimental because of drug-induced decreases in systemic blood pressure and associated decreases in coronary perfusion pressure.
Patients with severely impaired left ventricular function may not tolerate anesthesia-induced myocardial depression. Rather than volatile anesthetics, opioids may be selected for these patients. The addition of nitrous oxide, a benzodiazepine, or a low dose volatile anesthetic may be needed because total amnesia cannot be ensured with an opioid alone, but the addition of nitrous oxide or a volatile anesthetic may be associated with myocardial depression.
Hemodynamic goals for intraoperative therapy with β-blockers are unclear, and potential interactions with anesthetics that cause myocardial depression and vasodilatation must be considered. It seems prudent to maintain intraoperative heart rate at < 80 bpm.
Choice of muscle relaxant
The choice of nondepolarizing muscle relaxant in patients with ischemic heart disease is influenced by the impact these drugs could have on the balance between myocardial oxygen delivery and myocardial oxygen requirements. Muscle relaxants with minimal or no effect on heart rate and systemic blood pressure (vecuronium, rocuronium, cisatracurium) are attractive choices for patients with ischemic heart disease. Histamine release and the resulting decrease in blood pressure caused by atracurium are less desirable. Myocardial ischemia has been described in patients with ischemic heart disease given pancuronium, presumably because of the modest increase in heart rate and blood pressure produced by this drug. However, these circulatory changes produced by pancuronium may be useful for offsetting the negative inotropic and chronotropic effects of some anesthetic drugs.
Reversal of neuromuscular blockade with an anticholinesterase/anticholinergic drug combination can be safely accomplished in patients with ischemic heart disease. Glycopyrrolate, which has much less chronotropic effect than atropine, is preferred in these patients.
Monitoring
An essential prerequisite for the preservation of the balance between myocardial oxygen supply and demand is the establishment of a level of monitoring appropriate to the disease severity of the patient and the magnitude of the surgery. The following patient monitoring devices are essential to the safe conduct of anesthesia for all patients:
-
Electrocardiogram (ECG)
-
Noninvasive arterial pressure monitoring (NIBP)
-
Pulse oximetry (SpO2)
-
Capnography
-
Vapor analysis.
This level of monitoring is sufficient in the majority of patients with severe CAD undergoing low risk surgery but must be supplemented by additional monitoring for patients undergoing intermediate or high risk surgery:
-
Invasive cardiovascular monitoring
-
Temperature
-
Urine output.
Invasive cardiovascular monitoring includes arterial and central venous pressure monitoring. The use of pulmonary artery catheterization is controversial but is likely to be of benefit in the following groups of patients:
-
Patients with a recent myocardial infarction
-
Patients with significant CAD undergoing high risk surgical procedures
-
Patients with CAD and associated left ventricular dysfunction undergoing intermediate risk surgical procedures.
Intraoperative Management of Myocardial Ischemia
-
Methods of perioperative surveillance for myocardial ischemia include: computerised ST segment monitoring, pulmonary artery pressure monitoring and transoesophageal echocardiography. Computerised ST segment trend analysis is superior to visual interpretation of ST segment changes for the detection of intraoperative and postoperative myocardial ischemia and should be used if available. Similarly, changes in pulmonary artery pressure and pulmonary artery occlusion pressure and waveform can be sensitive indicators of myocardial ischemia. Transesophageal echocardiography, by the detection of wall motion abnormalities, is a further method in appropriately trained hands for the detection of intraoperative myocardial ischemia.
-
Inform the surgeon regarding the clinical scenario and plan with respect to stopping the surgery if possible or expedite the procedure.
-
The correction of hemodynamic status by manipulation of the depth of anesthesia and the use of vasoactive agents. β-blockers may be used to slow the heart rate and, thereby, to limit myocardial oxygen demand and increase myocardial oxygen supply. The rapid onset and titratability of the intravenous β-blocker esmolol make this a particularly suitable agent for use in this role.
-
Nitroglycerin is a more appropriate choice when myocardial ischemia is associated with a normal to modestly elevated blood pressure. In this situation, the nitroglycerin-induced coronary vasodilation and decrease in preload facilitate improved subendocardial blood flow but the nitroglycerin-induced decrease in afterload does not decrease systemic blood pressure to the point that coronary perfusion pressure is jeopardized.
-
Hypotension is treated with sympathomimetic drugs to restore coronary perfusion pressure. In addition to vasoconstrictor drugs, fluid infusion can be useful to help restore blood pressure. Regardless of the treatment, prompt restoration of blood pressure is necessary to maintain pressure-dependent flow through coronary arteries narrowed by atherosclerosis.
-
Institute invasive hemodynamic monitoring, if not done so far.
-
In an unstable hemodynamic situation, circulatory support with inotropes or an intra-aortic balloon pump may be necessary.
-
It may also be necessary to plan for early postoperative cardiac catheterization.
-
Shift the patient to coronary care unit or high- dependency unit after the surgery for postoperative management and follow-up.
Postoperative Care
The importance of continuing these principles of care into the postoperative period is increasingly apparent.
Numerous studies indicate that with modern anesthetic techniques, the occurrence of intraoperative myocardial ischemia can be limited, but that post-operative myocardial ischemia remains common and is associated with the development of significant cardiac morbidity and mortality. Proinflammatory responses initiated during the surgical procedure continue into the postoperative period and contribute to an increased risk of myocardial ischemia. Release of cytokines, the occurrence of hypercoagulability and diminished fibrinolytic activity, endothelial dysfunction and atherosclerotic plaque instability, hemodynamic changes, and increases in sympathetic nervous system activity associated with anesthetic emergence and suboptimal pain management have been identified as important factors mediating the increased incidence of ischemia postoperatively.
Postoperative care should concentrate on the maintenance of
-
adequate oxygenation
-
normothermia
-
hemodynamic stability requiring the continuation of invasive cardiovascular monitoring
-
fluid balance
-
appropriate pain control based upon regional anesthetic or systemic opioid analgesic techniques
-
administration of antiischemic medical therapy.
The appropriate location for such care is an intensive care or high dependency care environment. Sympathetic activation caused by postoperative pain is highly deleterious for the patient with coronary artery disease, and treatment of pain with intrathecal or epidural opioids with or without local anesthetics (ideally administered at the onset of the surgical procedure) or patient controlled analgesia is as essential to postoperative management as is continued administration of β-adrenoceptor antagonists.
Patients who require prolonged mechanical ventilation represent a special problem because typical sedatives/ hypnotics such as benzodiazepines may not eliminate sympathetic nervous system activation resulting from tracheal stimulation. Liberal use of systemic opioids (preferably morphine for additional cardioprotective benefits) may be required to attenuate this adverse
effect. Importantly, the severity of ischemic events can be profoundly diminished by adequate analgesia. β -agonists
may also find a role in the immediate postoperative period. The treatment of myocardial ischemia in the postoperative period may ultimately be more challenging than the intraoperative management.
